Advanced Medical Programs

Conditions We Specialize in Treating
-
Lumbar Spinal Stenosis
-
Persistent Low Back Pain
-
Persistent Neck Pain
-
Sciatica
-
Ankylosing Spondylitis
-
Persistent Shoulder Pain
-
Knee Osteoarthritis
All of these programs are designed and clinically tested by Dr. Carlo Ammendolia from the Mount Sinai Hospital in Toronto.
Do You Need a Chiropractor?
Eight out of ten Canadians will experience back and spine pain at some point in their lives. For many people, the pain can keep them from work, school, or from keeping up with their busy lives. Early treatment from a chiropractor can help get you back on your feet.
Your spine is one of the strongest parts of your body, but because it carries so much weight, it is also susceptible to injury. Accidents, stress, work poor posture, sports or sprains can cause back problems, When you injure your back, the pain can appear in other areas. Simple things like walking become painful with back injuries, and the changes we make in posture and stride can lead to pain in our hips, knees and feet.
Here are some symptoms of a back problem
- Leg pain with numbness, tingling, and/or weakness
- Back or leg pain when coughing or sneezing
- Difficulty standing up after sitting for any period of time
- Stiffness in the morning that decreases once you move around
- Pain in your hip, buttock, thigh, knee, or foot
- Inability to turn or bend to each side equally
- Unbalanced posture, when your head, neck, or shoulder may be higher on one side than the other
- Pain which prevents you from sleeping well
- Pain that persists or worsens after 48 hours
- Unable to walk distances
Chiropractors treat your back pain by addressing the cause of the pain. It’s simple , and it works
The word “chiropractic” combines the Greek words chiro (hand) and praxis (action) and means “done by hand.”
Chiropractic works because you are a self-healing, self-regulating organism, which is controlled by your nervous system. Signals and instructions flow from your brain, down the spinal cord and out to every organ, muscle, cell and tissue. Signals are then sent back to the brain to confirm if your body is working right. People of all ages are turning to chiropractic as a safe alternative to medications and surgery for acute and chronic pain.
You are healthier and pain free allowing you to live life to its fullest once again.
During your consultation, the doctor will ask you questions about your condition such as “Where does it hurt? What makes the pain better? What makes it worse? How bad is it and what else have you tried that hasn’t worked? We take physical rehabilitation very seriously. In fact, we focus on being the best at it. From the evaluation to the diagnosis and down to all our physical medicine treatments, you can be certain that you will be getting only the best care every step of the way.
A Healthy Spine is Essential for a Healthy Body
Chiropractic care is a drug-free, hands-on treatment that can immediately treat the source of your pain. Chiropractic adjustments allow the spine to return to its proper position and improve your overall range of motion. Chiropractic adjustments remove pressure from affected nerves allowing you to feel normal again. Studies show that chiropractic treatment is recognized as being a safe and effective treatment for most patients.
Conditions Common for Treatment
o Arthritis
o Shin Splints
o Fibromyalgia
o Runner’s Knee
o Wrist/Hand Pain
o Arm/Shoulder Pain
o Carpal Tunnel Syndrome
o Upper back pain
o Low back pain
o Sports injuries
o Sciatica
o Neck Pain
o Scoliosis
o Headaches/Migraines
o Patellofemoral Syndrome
o Thoracic Outlet Syndrome
o Motor Vehicle Accident injuries
o Achilles Tendinitis
o Plantar Fasciitis
o Tennis Elbow
Spinal Decompression
Spinal Decompression Therapy
Spinal Health and Rehabilitation Centre of Canada offers residents of Thunder Bay, Ontario and the surrounding area (or region) the latest cutting edge technology in the non-surgical treatment of serious lower back pain and sciatica. Our commitment to offering the highest quality of care resulted in the addition of the FDA cleared Spinal Decompression technology for the treatment of back pain. Spinal Decompression Therapy was developed to effectively treat lower back pain and sciatica resulting from herniated or degenerated discs, as well as Spinal Stenosis and/or Post-Surgical Pain Spinal Decompression Therapy, not only significantly reduces back pain in many patients, but also enables the majority of patients to return to more active lifestyles.
Nonsurgical Intervention
This clinical outcomes study was performed to evaluate the effect of spinal decompression on symptoms and physical findings of patients with herniated and degenerative disc disease. Results showed that 86% of the 219 patients who completed the therapy reported immediate resolution of symptoms, while 84% remained pain-free 90 days post-treatment. Physical examination findings showed improvement in 92% of the 219 patients and remained intact in 89% of these patients 90 days after treatment. This study shows that disc disease-the most common cause of back pain, which costs the health care system more than $50 billion annually, can be cost-effectively treated using spinal decompression. The cost for successful non-surgical therapy is less than a tenth of that for surgery. These results show that biotechnological advances of spinal decompression reveal promising results for the future of effective management of patients with disc herniation and degenerative disc diseases.
Spinal Decompression
Summary
In conclusion, non-surgical spinal decompression provides a method for physicians to properly apply and direct the decompressive force necessary to effectively treat discogenic disease. With the biotechnological advances of spinal decompression, symptoms were restored by subjective report in 86% of patients previously thought to be surgical candidates and mechanical function was restored in 92% using objective data.
ADVANCES IN BIOTECHNOLOGY
With the recent advances in biotechnology, spinal decompression has evolved into a cost-effective nonsurgical treatment for herniated and degenerative spinal disc disease, one of the major causes of back pain. This nonsurgical treatment for herniated and degenerative spinal disc disease works on the affected spinal segment by significantly reducing intradiscal pressures.1 Chronic low back pain disability is the most expensive benign condition that is medically treated in industrial countries. It is also the number one cause of disability in persons under age 45. After 45, it is the third leading cause of disability. 2 Disc disease costs the health care system more than $50 billion a year. The intervertebral disc is made up of sheets of fibers that form a fibrocartilaginous structure, which encapsulates the inner mucopolysaccharide gel nucleus. The outer wall and gel act hydrodynamically. The intrinsic pressure of the fluid within the semirigid enclosed outer wall allows hydrodynamic activity, making the intervertebral disc a mechanical structure. 3 As a person utilizes various normal ranges of motion, spinal discs deform as a result of pressure changes within the disc.4 The disc deforms, causing nuclear migration and elongation of annular fibers. Osteophytes develop along the junction of vertebral bodies and discs, causing a disease known as spondylosis. This disc narrows from the alteration of the nucleus pulposus, which changes from a gelatinous consistency to a more fibrous nature as the aging process continues. The disc space thins with sclerosis of the cartilaginous endplates and new bone formation around the periphery of the contiguous vertebral surfaces. The altered mechanics place stress on the posterior diarthrodial joints, causing them to lose their normal nuclear fulcrum for movement. With the loss of disc space, the plane of articulation of the facet surface is no longer congruous. This stress results in degenerative arthritis of the articular surfaces. 5 This is especially important in occupational repetitive injuries, which make up a majority of work-related injuries. When disc degeneration occurs, the layers of the annulus can separate in places and form circumferential tears. Several of these circumferential tears may unite and result in a radial tear where the material may herniate to produce disc herniation or prolapse. Even though a disc herniation may not occur, the annulus produces weakening, circumferential bulging, and loss of intervertebral disc height. As a result, discograms at this stage usually reveal reduced intradiscal pressure.
The early changes that have been identified in the nucleus pulposus and annulus fibrosis are probably biomechanical and relate to aging. Any additional trauma on these changes can speed up the process of degeneration. When there is a discogenic injury, physical displacement occurs, as well as tissue edema and muscle spasm, which increase the intradiscal pressures and restrict fluid migration.6 Additionally, compression injuries causing an endplate fracture can predispose the disc to degeneration in the future.
The alteration of normal kinetics is the most prevalent cause of lower back pain and disc disruption and thus it is vital to maintain homeostasis in and around the spinal disc; Yong-Hing and Kirkaldy-Willis7 have correlated this degeneration to clinical symptoms. The three clinical stages of spinal degeneration include:
1. Stage of Dysfunction. There is little pathology and symptoms are subtle or absent. The diagnosis of Lumbalgia and rotatory strain are commonly used.
2. Stage of Instability. Abnormal movement of the motion segment of instability exists and the patient complains of moderate symptoms with objective findings. Conservative care is used and sometimes surgery is indicated.
3. Stage of Stabilization. The third phase where there are severe degenerative changes of the disc and facets reduce motion with likely stenosis.
Spinal decompression has been shown to decompress the disc space, and in the clinical picture of low back pain is distinguishable from conventional spinal traction.8,9 According to the literature, traditional traction has proven to be less effective and biomechanical inadequate to produce optimal therapeutic results.8-11 In fact, one study by Mangion et al concluded that any benefit derived from continuous traction devices was due to enforced immobilization rather than actual traction.10 In another study, Weber compared patients treated with traction to a control group that had simulated traction and demonstrated no significant differences.11 Research confirms that traditional traction does not produce spinal decompression. Instead, decompression, that is, unloading due to distraction and positioning of the intervertebral discs and facet joints of the lumbar spine, has been proven an effective treatment for herniated and degenerative disc disease, by producing and sustaining negative intradiscal pressure in the disc space. In agreement with Nachemon’s findings and Yong-Hing and Kirkaldy-Willis,1 spinal decompression treatment for low back pain intervenes in the natural history of spinal degeneration.7,12 Matthews13 used epidurography to study patients thought to have lumbar disc protrusion. With applied forces of 120 pounds x 20 minutes, he was able to demonstrate that the contrast material was drawn into the disc spaces by osmotic changes. Goldfish14 speculates that the degenerated disc may benefit by lowering intradiscal pressure, affecting the nutritional state of the nucleus pulposus. Ramos and Martin8 showed by precisely directed distraction forces, intradiscal pressure could dramatically drop into a negative range. A study by Onel et al15 reported the positive effects of distraction on the disc with contour changes by computed tomography imaging. High intradiscal pressures associated with both herniated and degenerated discs interfere with the restoration of homeostasis and repair of injured tissue.
Biotechnological advances have fostered the design of Food and Drug Administration-approved ergonomic devices that decompress the intervertebral discs. The biomechanics of these decompression/reduction machines work by decompression at the specific disc level that is diagnosed from finding on a comprehensive physical examination and the appropriate diagnostic imaging studies. The angle of decompression to the affected level causes a negative pressure intradiscally that creates an osmotic pressure gradient for nutrients, water, and blood to flow into the degenerated and/or herniated disc thereby allowing the phases of healing to take place.
This clinical outcomes study, which was performed to evaluate the effect of spinal decompression on symptoms of patients with herniated and degenerative disc disease, showed that 86% of the 219 patients who completed the therapy reported immediate resolution of symptoms, and 84% of those remained pain-free 90 days posttreatment. Physical examination findings revealed improvement in 92% of the 219 patients who completed the therapy.
METHODS
The study group included 229 people, randomly chosen from 500 patients who had symptoms associated with herniated and degenerative disc disease that had been ongoing for at least 4 weeks. Inclusion criteria included pain due to herniated and bulging lumbar discs that is more than 4 weeks old, or persistent pain from degenerated discs not responding to 4 weeks of conservative therapy. All patients had to be available for 4 weeks of treatment protocol, be at least 18 years of age, and have an MRI within 6 months. Those patients who had previous back surgery were excluded. Of note, 73 of the patients had experienced one to three epidural injections prior to this episode of back pain and 22 of those patients had epidurals for their current condition.
Measurements were taken before the treatments began and again at week two, four, six, and 90 days post-treatment. At each testing point a questionnaire and physical examination were performed without prior documentation present in order to avoid bias. Testing included the Oswetry questionnaire, which was utilized to Surgical Alternatives: Spinal Decompression | ProAdjuster quantify information related to the measurement of symptoms and functional status. Ten categories of questions about everyday activities were asked prior to the first session and again after treatment and 30 days following the last treatment. Testing also consisted of a modified physical examination, including evaluation of reflexes (normal, sluggish, or absent), gait evaluation, the presence of kyphosis, and a straight leg raising test (radiating pain into the lower back and leg was categorized when raising the leg over 30 degrees or less is considered positive, but if pain remained isolated in the lower back, it was considered negative). Lumbar range of motion was measured with an ergonometer. Limitations ranging from normal to over 15 degrees in flexion and over 10 degrees in rotation and extension were positive findings. The investigator used pinprick and soft touch to determine the presence of gross sensory deficit in the lower extremities.
Of the 229 patients selected, only 10 patients did not complete the treatment protocol. Reasons for noncompletion included transportation issues, family emergencies, scheduling conflicts, lack of motivation, and transient discomfort. The patient protocol provided for 20 treatments of spinal decompression over a 6 – week course of therapy. Each session consisted of a 45-minute treatment on the equipment followed by 15 minutes of ice and interferential frequency therapy to consolidate the lumbar paravertebral muscles. The patient regimen included 2 weeks of daily spinal decompression treatment (5 days per week), followed by three sessions per week for 2 weeks, concluding with two sessions per week for the remaining 2 weeks of therapy. On the first day of treatment, the applied pressure was measured as one half of the person’s body weight minus 10 pounds, followed on the second day with one half of the person’s body weight. The pressure placed for the remainder of the 18 sessions was equivalent to one half of the patient’s body weight plus an additional 10 pounds. The angle of treatment was set according to manufacturer’s protocol after identifying a specific lumbar disc correlated with MRI findings. A session would begin with the patient being fitted with a customized lower and upper harness to fit their specific body frame. The patient would step onto a platform located at the base of the equipment, which simultaneously calculated body weight and determined proper treatment pressure. The patient was then lowered into the supine position, where the investigator would align the split of table with the top of the patient’s iliac crest. A pneumatic air pump was used to automatically increase lordosis of the lumbar spine for patient comfort. The patient’s chest harness was attached and tightened to the table. An automatic shoulder support system tightened and affixed the patient’s upper body. A knee pillow was placed to maintain slight flexion of the knees. With use of the previously calculated treatment pressures, spinal decompression was then applied. After treatment, the patient received 15 minutes of interferential frequency (80 to 120 Hz) therapy and cold packs to consolidate paravertebral muscles.
During the initial 2 weeks of treatment, the patients were instructed to wear lumbar support belts and limit activities and were placed on light duty at work. In addition, they were prescribed a nonsteroidal, to be taken 1 hour before therapy and at bedtime during the first 2 weeks of treatment. After the second week of treatment, medication was decreased and moderate activity was permitted.
Data was collected from 219 patients treated during this clinical study. Study demographics consisted of 79 female and 140 male patients. The patients treated ranged from 24 to 74 years of age (see Table 1). The average weight of the females was 146 pounds and the average weight of the men was 195 pounds. According to the Oswestry Pain Scale, patients reported their symptoms ranging from no pain (0) to severe pain (5).
RESULTS
According to the self-rated Oswestry Pain Scale, treatment was successful in 86% of the 219 patients included in this study. Treatment success was defined by a reduction in pain to 0 or 1 on the pain scale. The perception of pain was none 0 to occasional 1 without any further need for medication or treatment in 188 patients. These patients reported complete resolution of pain, lumbar range of motion was normalized, and there was the recovery of any sensory or motor loss. The remaining 31 patients reported significant pain and disability, despite some improvement in their overall pain and disability score.
In this study, only patients diagnosed with herniated and degenerative discs with at least a 4-week onset were eligible. Each patient’s diagnosis was confirmed by MRI findings. All selected patients reported 3 to 5 on the pain scale with radiating neuritis into the lower extremities. By the second week of treatment, 77% of patients had a greater than 50% resolution of low back pain. Subsequent orthopedic examinations demonstrated that an increase in spinal range of motion directly correlated with an improvement in straight leg raises and reflex response. Table 2 shows a summary of the subjective findings obtained during this study by category and total results post treatment. After 90 days, only five patients (2%) were found to have relapsed from the initial treatment program. Ninetytwo percent of patients with abnormal physical findings improved post-treatment. Ninety days later only 3% of these patients had abnormal findings. Table 3 summarizes the percentage of patients that showed improvement in physician examination findings testing both motor and sensory system function after treatment. Gait improved in 96% of the individuals who started with an abnormal gait, while 96% of those with sluggish reflexes normalized. Sensory perception improved in 93% of the patients, motor limitation diminished in 86%, 89% had a normal straight leg raise test who initially tested abnormal, and 90% showed improvement in their spinal range of motion.

10 tips for keeping your back healthy
- Exercise Regularly
- Follow a Healthy Diet
- Maintain good Posture
- Stretch your spine before and after sports
- Don't over load backpack or shoulder bag
- Stretch your legs and back after each hour of sitting
- Never cradle the phone between neck and shoulder
- Sleep on your back or side not your stomach
- Invest in a good chair, pillow, and mattress. It's worth it!
- See your chiropractor regularly
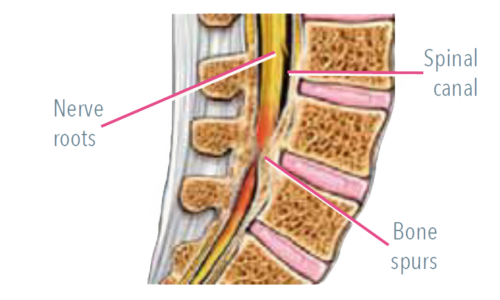
What is Lumbar Spinal Stenosis?
Lumbar spinal stenosis is a leading cause of pain, disability and loss of independence in older adults. It is usually caused by age-related arthritic narrowing of the spinal canals where nerves exit the spine travelling to the lower back and legs. This narrowing can cause compression of the spinal nerves leading to low back and leg pain, numbness, weakness, and reduced ability to stand and walk.
Decompression surgery to remove the bone and ligaments around the stenosis is an option for patients with severe symptoms.

Lumbar Spinal Stenosis Studies.
In an award-winning study, Ammendolia and Chow demonstrated the effectiveness of the Spinemobility Boot Camp Program for Lumbar Spinal Stenosis©.
PARTICIPANTS
49 individuals diagnosed with Lumbar Spinal Stenosis participated in the Study. At the baseline, participants were moderately to severely disabled, significantly limited in their walking ability and in moderate pain.
OUTCOME
Upon completion of the 6 week Spinemobility Program, participants exhibited clinically significant improvements in all outcome measures. These benefits were sustained over time, even after 3.5 years.
ODI Disability
Numeric Pain Score for Leg Pain
ODI Walk Score
Get Started
Click the link below book an appointment or simply learn more about our services.
BOOT CAMP PROGRAM
FOR LUMBAR SPINAL STENOSIS©
Coaching on behavioural change
Specific strategies for behavioural change and self-management for sustainable benefit

Targeted manual therapy
Condition-specific techniques to maximize spinal and neural mobility
Specific exercises & strength training
Targeted home exercises to maximize aerobic fitness, strength and flexibility
Body repositioning & self monitoring
Postural techniques to maximize standing, walking and functional abilities
The Chiropractic Advantage
Help For Your Back
Chiropractors are back specialists. Many medical doctors in Ontario refer patients with back pain to a chiropractor, and studies show that chiropractic treatment is increasingly recognized as the most safe and effective treatment for most patients with back pain
Chiropractic is a drug-free, hands-on treatment that can immediately treat the source of your back pain. Accidents, stress, or poor posture can injure your spine causing pain in the surrounding muscles, joints and nerves. Chiropractic treatment works because it treats the cause of your back pain, not just the symptoms.
How Does Chiropractic Work?
Your spine has a very important function in your body. Not only does it support your body’s weight, but it also protects your spinal cord, which is the “central highway” of your nervous system. Our ability to walk, run, jump, lift and feel almost every sensation below your neck requires a healthy spine.
Chiropractors Understand How to Relieve Pain.
The bones in your back, called the vertebrae, are connected by cartilage and work together in a very specific way. When everything is working well, your spine is in line, strong and flexible. The stress of daily living, injuries, or accidents can cause the bones to shift out of their proper alignment or affect their range of motion. These small changes can cause pain by putting pressure on the different joints, muscles, and nerves along your spine.
Chiropractors understand how to relieve this pain. They are specially trained to find the source of your back pain, assess the problem, and make the proper adjustments that allow your spine to work properly again. Chiropractors might also use massage, ultrasound, exercise or other therapies to treat your back problem.
It's Simple Treatment That Works
Chiropractic joint manipulation or “adjustment” is a treatment where the Chiropractor uses his or her hands to apply a very quick, precise, and safe amount of pressure directly on the problem area of your spine. This pressure momentarily separates the joints, allowing a gas bubble to escape (this is the popping sound or cracking noise you might have heard about). This relieves the pressure on the joint and surrounding nerves, allowing your spine to return to its proper position. The adjustment is not painful and often provides immediate relief. It’s a simple treatment that works.
Our Machines
Lumbar Extension Machine
The MedX Lumbar Extension machine provides functional testing and spinal therapy. A unique system of pelvic stabilization provides true isolation of the deep muscles of the lumbar spine (erector spinae and multifidus) weakness of these muscles can be responsible for chronic disability and recurring pain.
Cervical Extension Machine
The MedX Cervical Extension machine is highly reliable and specific for the quantification of isometric cervical extension strength and dynamic variable resistance training.
Because the cervical muscles continual support the weight of the head, headache, and neck pain are common complaints.
These machines are used in all of the professional sports facilities including the NFL, NHL, NBA and other professional sports training facilities to maximize their athlete’s performance.
Having an exceptionally strong core muscle group is critical to spinal stability. Having a strong cervical spine allows you to have maximum head and neck support which is critical with todays’ technology and daily living activities.

